Health
New report aims to help evaluate critical LGBTQ+ health data collection
The report provides the NIH with guidance for gathering data on gender and sexuality, key to understanding disparities across marginalized populations.

This story was originally published by The 19th
 A groundbreaking report by the National Academy of Sciences on how to best gather information on gender and sexuality says gender identity, not biological sex, should be the default data collected and reported.
A groundbreaking report by the National Academy of Sciences on how to best gather information on gender and sexuality says gender identity, not biological sex, should be the default data collected and reported.
The report, released this month, provides recommendations to the National Institutes of Health for how to measure gender and sexuality throughout different health contexts, including in research, surveys, health care administration and clinical practice. Made up of 27 different branches, the NIH is the nation’s agency for medical research, as well as the largest funder of biomedical research in the world. Its global influence puts it in a unique position to model meaningful data collection on gender and sexual minority populations.
Accurate data collection is essential to understanding disparities across marginalized populations. Integrating these new metrics will help research programs better evaluate the specific health needs of LGBTQ+ populations.
LGBTQ+ communities have rarely been represented in general population surveys. This is the first rigorous study of how or when data on sex, gender or sexuality should be collected. Without a universal standard, data cannot be combined or compared accurately. For instance, one survey may have asked about gender and another about sex, and thus they ended up measuring different things.
The report, funded by the Department of Health and Human Services, includes suggested language for survey questions, which data should be collected in which context, and extensive research on privacy concerns and how to minimize potential harm while collecting data. Nancy Bates, retired senior methodologist for survey research at the U.S. Census Bureau and co-chair of the committee that wrote the report, told The 19th in email that the nine-member committee was made up of researchers who identified across the gender and sexuality spectrum, specifically including two-spirit (a general term to describe the variety of culture-specific Indigenous genders and sexualities), intersex and gender nonconforming identities.
Overall, the report emphasizes capturing identity over biology and highlights the potential for discrimination if data isn’t collected in an organized, thoughtful way. Because these aspects identify marginalized populations, there is an inherent risk in collecting the data in the first place. To minimize discrimination and misuse, not all data is recommended to be collected in every context.
Many surveys conflate sex and gender, confusing both survey respondents and the analysts trying to draw meaningful conclusions from the data. The report defines sex as a grouping of biological characteristics, while gender encompasses identity and expression. The panel recommends collecting data on sex only in situations where it is explicitly required, like when a doctor is trying to schedule a Pap smear or prostate exam. This ties into the core recommendation to collect only the minimum amount of data necessary.
The report lays out a two-step protocol for classifying gender identity: Respondents are asked about the sex on their birth certificate and their current gender identity. Past research has shown that asking about only gender identity has led to undercounts of the transgender population. For example, maybe one transgender woman would identify her gender as transgender, and another would identify her gender as female. The two-step method ensures both are classified as people with “transgender experience,” which is relevant data in some contexts.
There are also strict privacy protections around how the data is reported, accessed and used. Many LGBTQ+ people have suffered when their identities have been involuntarily disclosed, and professional groups have highlighted the potential dangers of gathering sensitive data on marginalized populations. The authors conclude that population-level data-gathering is unlikely to result in direct harm to individuals.
The authors note that the most likely harm to come through this method of aggregate data collection is that the insight or benefits provided never make it back to the community in question. They highlight best practices for sharing research findings with the communities participating in a study.
The panel’s recommended language for gender identity includes named options for only male, female and transgender. The limited options were chosen purposefully to prioritize aggregation; given the sample sizes of many surveys, if more specific options were included (e.g. “transgender male-to-female”) there likely would not be enough responses to both give meaningful insight and protect the privacy of respondents.
A significant part of the report is dedicated to the design of standardized questions about gender, sex and sexuality. The final options for gender include male, female, transgender and two-spirit (a generalized Western term meant to refer to Indigenous identities outside of the gender binary). However, the option for two-spirit on both the sexuality and gender identity questions will appear only if the respondent has selected “American Indian or Alaska Native” as their race.
The decision to show two-spirit as an option for only Indigenous people is rooted in both cultural competency and data quality. (Bates explained that the committee consulted with Indian Health Services about how to collect data on two-spirit individuals.) As part of the research for this report, a sample of survey questionnaires were evaluated to inform potential language and question design. One of those was the All of Us Survey, an NIH research program gathering diverse health information. All of Us included two-spirit as an option for gender, and an analysis of responses found that over two-thirds of people who identified as two-spirit did not identify as Indigenous. Restricting the choice ensures data on Indigenous populations is being accurately collected.
Another new area of focus detailed in the report is data collection for intersex populations. Little data is available on intersex individuals or people who have been diagnosed with disorder of sex difference (DSD). There has yet to be a federal population survey in the United States that includes questions on intersex status, and the most comprehensive survey of intersex adults was fielded just two years ago.
Intersex, or DSD, is a broad term that includes anyone born with characteristics of both sexes. Because of the varying nature of the designation and how it usually is based on clinical data, many people may not know whether they are intersex, which complicates data collection. Further, many hospitals historically have performed genital surgery on intersex newborns under the auspices of aligning a child to a binary sex — not always with the knowledge or consent of the parents. In this way too, it’s possible for someone to not know they are intersex. California is the only state to have condemned unnecessary genital surgery in children.
The panel recommends the collection of data on intersex traits in clinical settings where sex characteristics are needed to determine course of care. Bates said the committee took into account recommended measures jointly developed by the Fenway Institute and InterAct Advocates For Intersex Youth. However, they note that more research on the phrasing of questions is necessary. Notably, it is recommended that a question about intersex status be separate as opposed to included as an option for sex or gender. This is another example of how the report emphasizes the decoupling of social identity and biological characteristics.
A representative from NIH’s Sexual & Gender Minority Research Office told The 19th that their office is in the process of sharing this information across the organization and the Department of Health and Human Resources. In a public statement shared upon the report’s release, Dr. Lawrence A. Tabak, acting director of the NIH, shared the potential impact on all federal programs. “I hope that this report will facilitate the collection of sex, gender identity, and sexual orientation across the broader federal landscape.”
The 19th is an independent, nonprofit newsroom reporting at the intersection of gender, politics and policy.
Mental Health
Gender dysphoria is a protected disability, federal appeals court finds
Experts say the opinion gives transgender people a powerful tool to advocate for their rights in workplaces, prisons, schools and hospitals.

This story was originally published by The 19th
 The Americans with Disabilities Act (ADA) extends protections to people with gender dysphoria, a federal appeals court found this week. The opinion, issued Tuesday, marks the first time any federal appellate court has considered whether gender dysphoria — distress experienced by many, but not all, transgender people due to their body not aligning with their gender — should be a protected disability under the ADA.
The Americans with Disabilities Act (ADA) extends protections to people with gender dysphoria, a federal appeals court found this week. The opinion, issued Tuesday, marks the first time any federal appellate court has considered whether gender dysphoria — distress experienced by many, but not all, transgender people due to their body not aligning with their gender — should be a protected disability under the ADA.
The opinion enables trans people living with gender dysphoria to use federal disability laws to protect them if they live in states covered by the U.S. Court of Appeals for the Fourth Circuit — Maryland, Virginia, West Virginia, North Carolina and South Carolina. Other courts could agree with the precedent, although they’re not obligated to do so.
The details of the case brought to the court dealt with abuse that trans prisoners face behind bars in the United States, often because they are not housed according to their gender identity. But, experts say, the consequences of the opinion are far-reaching and give trans people a new powerful tool in fights over their civil rights — in workplaces, prisons, schools and hospitals.
Protection under the ADA is a powerful tool because of how the law requires reasonable accommodations for people with disabilities — it doesn’t just mandate non-discrimination. That opens up a world of possibilities for lawsuits brought against anti-trans discrimination, possibilities that go beyond what the Equal Protection Clause, Title VII or Title IX can offer, experts say.
“This really is a landmark case. It’s probably been over two decades in the making by lawyers, trans lawyers, trans clients [and] advocates,” said Kevin Barry, interim dean and law professor at Quinnipiac University School of Law.
Protections granted under the ADA for trans people with gender dysphoria may look like getting a week off from work while recovering from gender-affirming surgery, or taking the morning off for counseling related to gender transition, Barry said. Trans prisoners in particular face “horrific discrimination” when trying to access hormone therapy, surgery or correct housing, he said — and being able to make a claim under the ADA grants them a new avenue to make a case for those rights.
Tuesday’s decision by the Fourth Circuit stemmed from a lawsuit brought by Kesha Williams, a trans woman who says that prison staff harassed her, misgendered her, denied her hormone treatment and improperly housed her with men while she was incarcerated in a Virginia detention center. The Fairfax County Sheriff’s Office in Virginia, which oversees the detention center that Williams was held in, declined to comment, citing the ongoing litigation.
The federal appeals court reversed the previous dismissal of Williams’ ADA claims and sent her case back to the United States District Court for the Eastern District of Virginia. The state can petition for a full court rehearing in front of the Fourth Circuit, or Virginia could ask the Supreme Court to review whether the federal appeals court decision was correct.
“But right now, we have the law of the land in the Fourth Circuit, at least,” said Chris Erchull, staff attorney at GLBTQ Legal Advocates & Defenders (GLAD).
Trans people who want to be considered protected under the ADA must show that they are being medicated for gender dysphoria. And while not all trans people experience that dysphoria, or are able to access gender-affirming care, it is still a significant win for trans rights, and for attorneys that have been making this same argument — and winning cases based on this argument — in courts across the country for years.
Lawyers bringing disability discrimination claims for clients with gender dysphoria are not arguing that being transgender is a disability, or that being trans reflects on anyone’s ability to accomplish certain things, Erchull said.
“What we do mean to say is that people with gender dysphoria experience prejudice, are subject to stereotypes and live in a world that’s not accommodating,” he said.
The argument that ADA protections cover transgender people notched its first legal win in 2017, when a federal district court in Pennsylvania recognized gender dysphoria as a disability under the ADA. That case followed years of pressure from lawyers and advocates, said Barry, who worked on the ADA Amendments Act of 2008 to broaden protections and include transgender people. The arguments go as far back as 2002, when Jennifer Levi at GLAD made the first case arguing for a trans client to be covered under Massachusetts’ law against disability discrimination, Barry and Erchull noted.
The Williams decision is orders of magnitude more impactful than that 2017 case, because it binds all district courts in the Fourth Circuit, Barry said. The decision should also provide precedent to other circuit courts across the country.
Joshua Block, senior staff attorney with the ACLU’s LGBTQ & HIV Project, said the precedent set by this decision could aid legal fights over states attempting to enact gender-affirming health care bans or exclusions — especially due to how some states try to split hairs on who their laws are actually affecting.
“A fight that we constantly have … is we say, by excluding this health care, you’re discriminating against trans people. And they say, no we’re not discriminating based on trans status, we’re just discriminating based on this diagnosis of gender dysphoria. And if the ADA applies, then that’s not a viable response … because it’s a protected disability,” he said.
The Fourth Circuit court’s decision is also significant within the world of disability law, said Doron Dorfman, associate professor at Seton Hall Law School, who specializes in disability and health law. Strongly connecting gender dysphoria to impairment, as it’s used in disability law to guarantee protections for people living with disabilities, is a tactic he has not seen used much in cases backing transgender rights.
“This decision affirms the rights of transgender people with gender dysphoria, in our rights under federal disability laws,” said Ezra Ishmael Young, who teaches constitutional law at Cornell Law School.
In a statement, Williams’ attorney, Joshua Erlich, noted that the court’s holding applies to anyone seeking accommodations for gender dysphoria in employment or other contexts, and said: “We’re thankful that the Fourth Circuit ruled in her favor and we are excited to get back into court to vindicate Kesha’s rights.”
The 19th is an independent, nonprofit newsroom reporting at the intersection of gender, politics and policy.
Medical
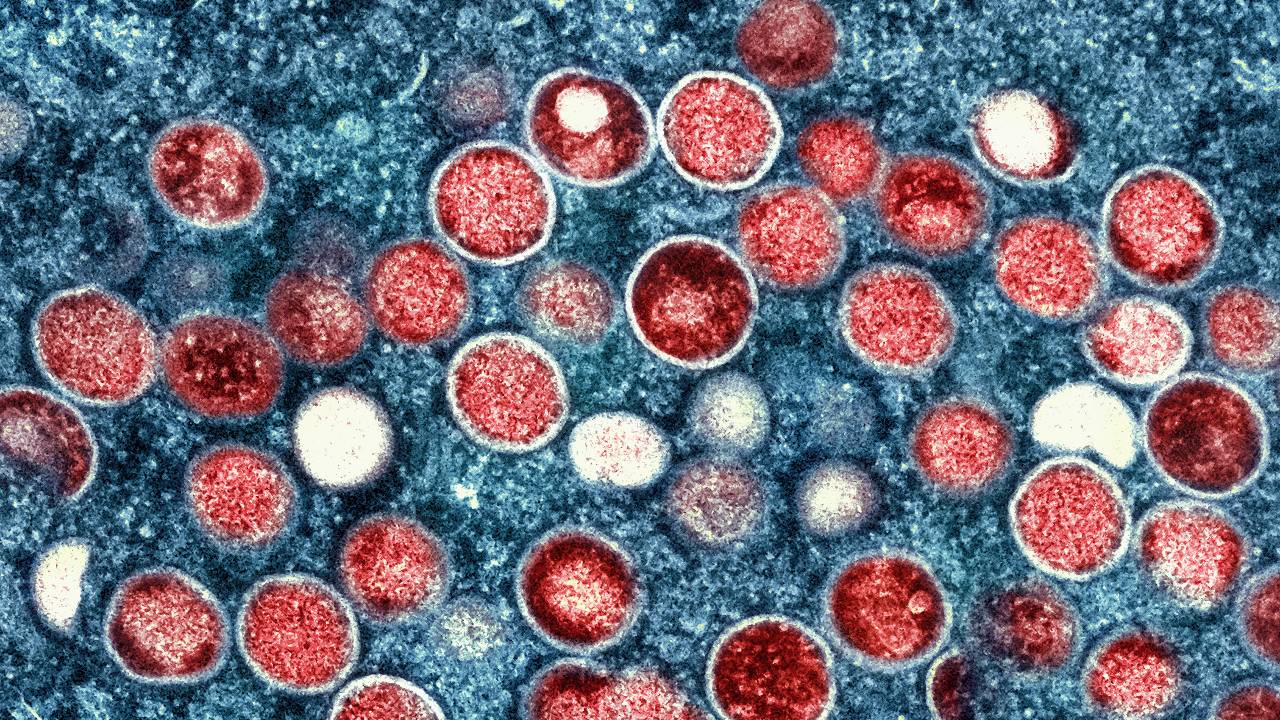
Experts debunk monkeypox myths as misinformation spreads
Can monkeypox spread on the subway? Can it kill like COVID-19? Experts respond to monkeypox myths and misconceptions.
This story was originally published by The 19th
 Can monkeypox spread on the subway? Can it kill like COVID-19? Is it transmitted through sex?
Can monkeypox spread on the subway? Can it kill like COVID-19? Is it transmitted through sex?
Misconceptions, myths and a lack of public knowledge on the monkeypox virus are widespread. Despite 57 percent of adults recently polled by Morning Consult feeling confident in the Centers for Disease Control and Prevention’s ability to control the spread of monkeypox, many Americans are misinformed on how the virus spreads and how concerned they should be right now — as they face the virus for the first time.
Last month, the Annenberg Public Policy Center found that nearly half of 1,580 surveyed adults were not sure if monkeypox was less contagious than COVID-19. (It is much less contagious.) One-third of more than 4,000 adults polled by Morning Consult aren’t sure how monkeypox spreads. Two-thirds of those surveyed by Annenberg were unsure or didn’t believe that there is a monkeypox vaccine (there is, it’s FDA-approved, and to be eligible for a vaccine right now in most areas, people must be in a high-risk group — predominately queer men, or trans and nonbinary people, who have had multiple or anonymous sex partners in the last two weeks.).
Monkeypox is a disease primarily transmitted through skin-to-skin contact that can infect anyone, but is currently affecting queer men the most.
Here’s what experts have to say in response to common misconceptions and myths about the monkeypox virus.
People can get monkeypox on public transit, in dressing rooms, or while shopping: False
The risk of getting infected through these situations is extremely low, said Stephen Abbott, medical director at Whitman-Walker’s Max Robinson Center, a D.C.-based healthcare provider focused on serving LGBTQ+ people.
Abbott stressed that spread occurs through direct skin-to-skin transmission — not skin-to-object, then someone else touching that object. The virus can spread by touching sex toys, sheets and other fabrics that have made contact with exposed lesions or skin rashes, per the CDC — but the vast majority of cases are being reported by men who had sex or close intimate contact with another man prior to infection.
Places where a person could typically pick up a cold or flu virus are not considered primary points of transmission.
“There’s really no evidence at this time to suggest people are being infected through casual contact through public transportation, and anything like that. The vast majority of the cases that have been identified from the outbreak so far had been through intimate contact or sexual activity,” said Daniel Uslan, co-chief infection prevention officer at UCLA Health and clinical chief of infectious diseases.
Monkeypox can spread through shaking hands or hugging: Not likely
These are also very low-risk situations, Uslan said, adding that he is not aware of recorded cases where handshaking is the suspected route of transmission.
But skin-to-skin contact with someone who has an open lesion can still occur if those lesions are on the hands, Abbott noted — and some lesions are so small that patients don’t notice them.
“Some of the patients I’ve seen when I do their skin exam, they haven’t even noticed that they have a lesion on their hand,” he said. “They might inadvertently shake someone’s hand and expose them unknowingly.”
However, some of the fears surrounding the spread of monkeypox — especially from low-risk encounters in public spaces — seem to manifest from anti-LGBTQ+ sentiment, as gay and bisexual men are primarily contracting the virus right now, said Perry Halkitis, dean and professor of public health and health equity at Rutgers School of Public Health.
“People will use any piece of information, if they are homophobic, to disadvantage and to stigmatize gay men,” he said.
Monkeypox is an STD or STI: False, but sexual contact is still driving the spread.
The virus can spread through any prolonged skin-to-skin contact with lesions or rash areas — but transmission during sex, where plenty of skin-to-skin contact takes place, is still primarily how the virus is spreading right now.
“You can have sex with somebody and have the flu, and they can get the flu. That doesn’t make the flu an STI,” Halkitis said. Oral, anal, or vaginal intercourse are not required for monkeypox transmission to occur, he added.
“Technically, it is not [an STD or STI] because it is not solely spread through sexual contact. But the current outbreak appears to be spreading primarily through sexual contact, so it is associated with sex, but is not technically a sexually transmitted infection,” Uslan said.
Abbott agreed that, by definition, monkeypox is not an STI or STD. Josh Michaud, associate director of global health policy at the Kaiser Family Foundation, noted that the answer should ultimately not affect how the country responds to the virus — and that labeling the virus as an STI may not be black or white.
“What we know is that sexual behavior, or particularly men who have sex with men with multiple partners, has been the bulk of the cases so far of monkeypox. And therefore transmission is very much associated with sexual activity,” Michaud said. “I think people are sort of debating terminology here. And we don’t necessarily need to classify it to be able to respond to it one way or the other.”
Having chickenpox or shingles protects someone from monkeypox: False
The virus that causes chickenpox is unrelated to monkeypox, although their names are similar.
“The viruses are in completely different families,” said Michaud. “In the case of the chickenpox virus, it doesn’t provide any cross-protection against monkeypox.”
Getting the smallpox vaccine as a kid protects against monkeypox: Likely
Someone who got the smallpox vaccine as a kid would likely have some protection against current monkeypox transmission, experts say, since the viruses are in the same family. However, any immunity provided by a childhood smallpox shot may have waned.
“Health departments are still suggesting that those folks get vaccinated,” Abbott said, adding that immunity may have waned because smallpox was declared eradicated in 1980.
The passage of several decades since smallpox vaccinations were commonplace means that most young people have not received the same level of protection, Uslan noted.
Monkeypox is as contagious, or as dangerous, as COVID-19: False
Monkeypox is not as contagious, or as fatal, as COVID-19, which is highly transmissible through airborne and respiratory routes.
“It is absolutely not as contagious as COVID,” Uslan said. Monkeypox is not spreading through casual contact, and evidence so far shows that patients are not contagious with monkeypox until symptoms emerge — as opposed to COVID-19, which asymptomatic people can spread.
“It’s also not nearly as fatal,” Abbott said, and it won’t leave you with a chronic infection. “It’s a rash that is very uncomfortable and painful. But most people will recover in two to four weeks.”
While scarring can be one long-term side effect, after the lesions heal, there haven’t been reports of a “long” monkeypox syndrome similar to the long COVID that many Americans have experienced.
People are at higher risk of contracting monkeypox if they’ve had COVID-19 before: False
There is no evidence to suggest that getting COVID-19 increases a person’s risk to contract monkeypox. While those who are immunocompromised are more susceptible to contract a variety of viruses, Halkitis noted, contracting COVID does not mean someone is more likely to get monkeypox.
“With two different diseases, one doesn’t create exposure to the other,” Abbott said.
Children are at risk of getting monkeypox right now: False
Children are still at minimal risk. While the virus could spread into their social networks at some point, the current focus to slow the spread of the virus is to vaccinate men who have sex with men.
“I don’t think parents should be terribly worried at this time, but this is something that people should be paying attention to,” Uslan said. “We have not seen a lot of cases in daycare settings for children at this point. So it doesn’t seem to be a major concern.”
While a few monkeypox cases have been seen in women and children, and the potential for greater spread cannot be ignored, the difference in risk right now is still massive, Michaud said.
Everyone is at the same risk of getting infected right now: False
A person’s risk of getting infected with monkeypox is high right now if they are among high-risk groups like queer men who have recently had multiple sexual partners or anonymous sex, or aren’t using protection.
“If we’re gonna get ahead of this and keep it from escalating, we need to be vaccinating those at highest risk — gay and bisexual men and our networks, and trans folks as well,” Abbott said, noting that social networks within these groups can be vectors for spread alongside sexual networks.
“The highest-risk individuals in my view are young gay and bisexual men, born after 1972, who have no smallpox vaccination, and who are socializing in large groups with other gay men,” Halkitis said.
It’s not safe for people with eczema to get the JYNNEOS vaccine shot: False
It’s safe to get the JYNNEOS shot even with eczema or similar skin conditions. However, ACAM2000, an FDA-licensed smallpox vaccine that may also be effective against monkeypox but is not being widely offered due to a long list of side effects and a more difficult injection procedure, can be harmful to those with eczema and those with other exfoliative skin conditions or dermatitis.
TPOXX treatment is not safe for people living with HIV: False
TPOXX, the antiviral and primary pain management treatment for monkeypox,is safe for those living with HIV, including those taking antiviral drugs to manage their HIV, experts said. There are also no interactions between the JYNNEOS vaccine and HIV medications, Halkitis said.
More studies on TPOXX’s effectiveness are gearing up and are likely to start in the next few weeks, Uslan said, although it is already known that the treatment is safe and well-tolerated in healthy patients.
According to an analysis by the CDC of monkeypox cases from May through July, a substantial number of monkeypox cases have been reported among those with HIV.
Find more information on monkeypox symptoms, how the virus spreads, and what to do if you are sick from the CDC’s website.
Disclosure: Pfizer, CVS Health, the Human Rights Campaign, and the chairman of Enterprise Product Partners, Randa Duncan Williams, have been financial supporters of The 19th.
The 19th is an independent, nonprofit newsroom reporting at the intersection of gender, politics and policy.
Mental Health
Survey: Mental Health Concerns Increase Among All Americans
Fifth survey since April 2020 tracks mental health impact of pandemic on ages 18+ and the utilization of new technology and tools to meet demand for support

WOONSOCKET, R.I. — A recent CVS Health®/Morning Consult survey of Americans age 18+ found that mental health concerns are continuing to rise among individuals of all backgrounds, especially Black, age 65+, young adult, and LGBTQIA+ respondents. The survey also found more Americans agree that the pandemic has made them more comfortable seeking support for mental health and using technology to address it.
Key findings include:
- Six-in-ten (59%) Americans have experienced concerns about either their own mental health or that of family and friends, a 9%-point increase since April 2020.
- More than half of Americans (53%) agree that hearing about other people’s challenges makes them more comfortable seeking out resources and care for themselves.
- Since the pandemic began, most people agree that society has become more comfortable engaging in mental health discussions (56%), using digital tools to improve mental health (58%) and using telemedicine for therapy (63%).
The growing use of telemedicine and digital tools to treat mental health increases access to care, allows for greater convenience in connecting with a mental health provider, and can be a welcome option for those who are apprehensive about receiving mental health care in person.
“Despite the longstanding stigma and other challenges in mental health, there is a clear shift taking place through the power of technology,” said CVS Health President and CEO Karen S. Lynch. “CVS Health provided 10 million virtual mental health visits last year, compared to 20,000 prior to the pandemic, which is enabling us to meet the growing demand brought on by COVID-19. We are firmly committed to developing new programs and resources that help make mental health care more routine, convenient and accessible for all communities.”
Some are Suffering More than Others
The survey found the LGBTQIA+ community, young adults, Blacks, and respondents age 65+ had greater increases in mental health concerns:
- 57% of respondents who identify as LGBTQIA+ expressed concerns about their own mental health, 20%-points higher compared to other respondents.
- 74% of respondents aged 18-34 experienced mental health concerns for themselves, family or friends, reflecting a 12%-point increase compared to two years ago.
- Black Americans surveyed saw an 11%-point increase in mental health concerns since the start of the pandemic.
- Four-in-ten respondents age 65+ experienced mental health concerns for themselves, family or friends, reflecting a 10%-point increase compared to two years ago.
The survey also found that while 74% of employed adults agree that employers should offer their employees resources and access to mental health services, only 35% of employed adults feel comfortable discussing mental health with a colleague, indicating an opportunity for workplaces to further engage their employees.
“The impact of isolation, loss, grief and burnout will effect of our mental health for years to come,” said Cara McNulty, President, Behavioral Health and Mental Well-being, CVS Health. “As a result, we continue to expand services and resources to meet the long-term needs of communities, workforces – including our own – and loved ones to make gains on our goal to reduce suicide attempts 20 percent among our membership by the year 2025, which is an imperative.”


